Spinal Cord Injury Awareness Month: Research Roundup
September is National Spinal Cord Injury Awareness Month. The IDEAL RRTC rounds up recent research from our faculty contributing to a growing body of knowledge on the long term health and wellbeing of SCI survivors.
Every September, organizations like United Spinal Association and Project 34 and individuals celebrate Spinal Cord Awareness Month highlighting the diverse experiences of individuals with spinal cord injuries (SI) and raising awareness of many barriers that individuals with SCI must overcome to live healthy lives.
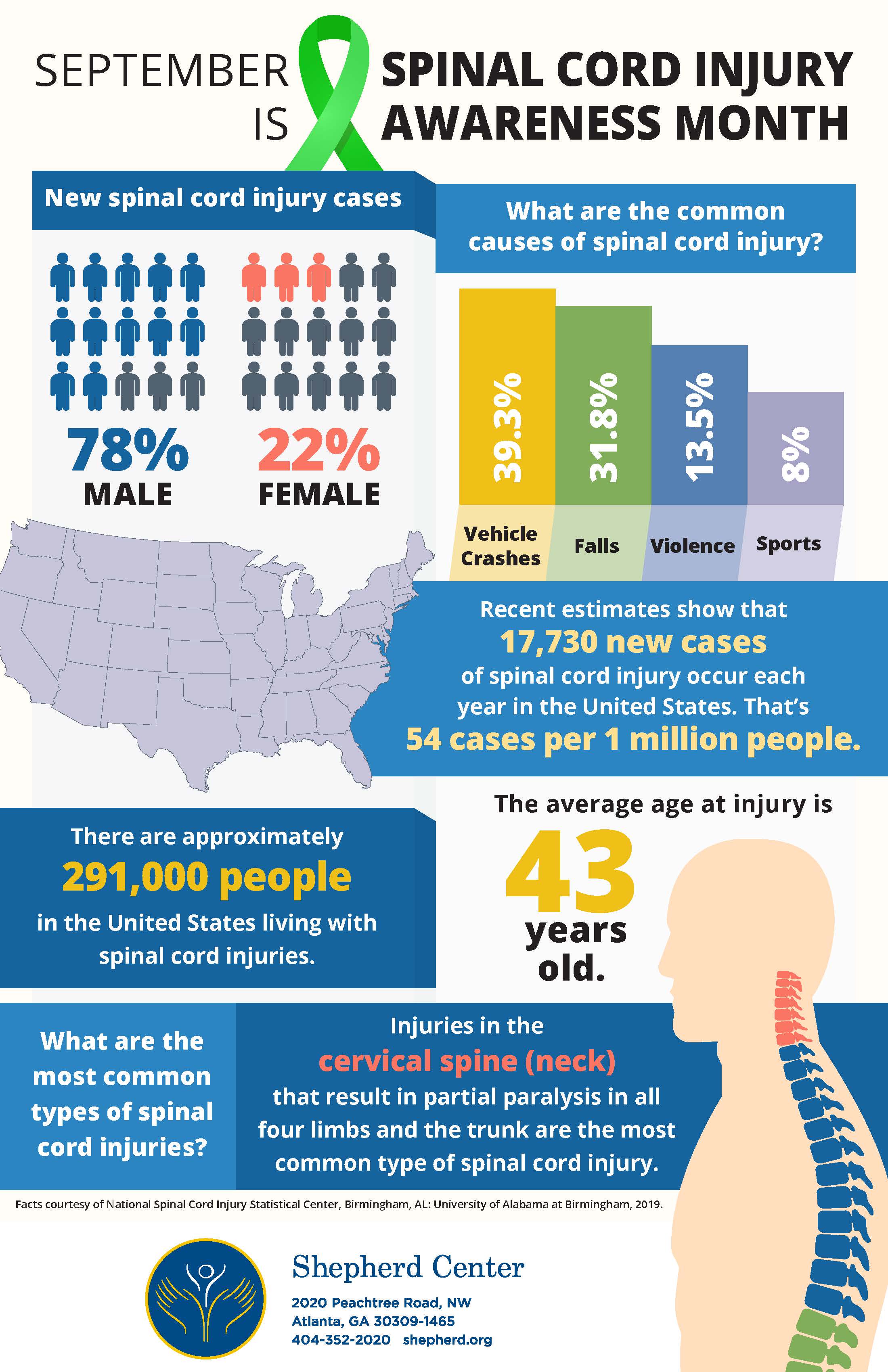
According to the National Spinal Cord Injury Statistical Center’s “Facts and Figures at a Glance 2020" (PDF), there are approximately 294,000 Americans currently living with spinal cord injuries (SCI), and 17,810 new cases each year. Additionally, spinal cord injuries disproportionately affect Black Americans, who sustain approximately 24 percent of injuries, despite being only 13 percent of the general population. Vehicle crashes are the most recent leading cause of injury, closely followed by falls and acts of violence, primarily gunshot wounds. Sports and recreation activities are also relatively common causes.
Individuals living with SCI face unique challenges to healthy aging, including higher rates of unemployment and higher risk for both acute and chronic health issues like depression, genitourinary diseases, chronic pain, and respiratory issues. Since 2015, about 30% of persons with SCI are re-hospitalized one or more times during any given year following injury. Among those re-hospitalized, the length of hospital stay averages about 18 days. The average life expectancy for people after they sustain SCI have not improved since the 1980s and rates remain significantly below life expectancies for people without SCI.
Several IDEAL RRTC researchers study the long-term impact of SCI on individual health and wellbeing, as well as the economic and system-level cost of SCI in the American health care system. Here’s a roundup of recent IDEAL RRTC-authored SCI research:
Individuals with SCI are at higher risk chronic conditions like depression and anxiety, substance use disorder, chronic pain, and dementia
A 2019 analysis published in The Spine Journal found that of private insurance records found that adults with non-traumatic spinal cord injuries had a higher prevalence of many psychological morbidities, including adjustment reaction, anxiety disorders, depressive disorders, drug dependence, episodic mood disorders, central pain syndrome, psychogenic pain, dementia, and multimorbidity, as compared to adults without a SCI.
The research team, led by Mark Peterson, Ph.D. highlight the need for early detection and services that help individuals with SCI reduce their risk of disease onset and help patients slow the progression of secondary conditions.
Article Citation: Peterson MD, Kamdar N, Whitney DG, Ng S, Chiodo A, Tate DG. Psychological morbidity and chronic disease among adults with nontraumatic spinal cord injuries: a cohort study of privately insured beneficiaries. The Spine Journal. 2019;19(10):1680-1686. Doi: 10.1016/j.spinee.2019.05.591.
Adapting to work after SCI
Conducting small focus groups with 44 individuals with SCI, this study identified challenges that individuals with SCI face in getting back to work. This paper revealed the physical health and functioning issues that individuals had to consider when adapting to work after SCI and in their decision to continue work or to change or discontinue employment. Here are some quotes from the focus groups:
"Relearning one’s body and the day-to-day: “I remember vividly 25 years ago, it took me 2 or 3 hours to get up and dressed, an hour to get downtown, 11 o'clock, and so tired after 2 o'clock, went back home. In that transition, you don't know if you're going to work or not, do you want or not want to work, are your skills the same in the chair? There are a lot of things you have to look at.”
The vulnerability of functioning in a work environment after SCI
"Asking a stranger to help you. I said to my therapist I ride Metro Mobility for the last 21 years. I would have to say there have been over a thousand plus men who have been driver who have come close enough putting belts over me and touching my chair. I would never as an able-bodied person run into a thousand men that I would have allow that interaction. And now I have to allow that to get from one place to the other. Have their comments, and can I get away from someone who has just belted me down with five belts. As a single, able-bodied woman, would you ever have had to ask a stranger to help you that way?...And have to trust them and be that close to be vulnerable."
Aging, functioning and leaving the workforce
“Everything took longer. My shoulders are shot and a myriad of other things. It got more difficult. That's why I hung it up. Plus I wanted to work until 66 just because I wanted to do that to fulfill my work life because that's where I came from. But anyway, it just became difficult. Life is very hard. Now everything takes longer.”
The research team, led by Michelle Meade. Ph.D., note that learning to manage health after SCI can be a long and complicated process that is dependent on numerous personal and environmental factors. They hope that the themes identified through the study might serve as a starting point for the development of interventions to enhance employment outcomes after SCI.
Article Citation: Meade MA, Reed KS, Krause JS. The Impact of Health Behaviors and Health Management on Employment After SCI: Physical Health and Functioning. Topics in Spinal Cord Injury Rehabilitation. 2016;22(1):39-48. doi:10.1310/sci2201-39. (Open Access)
Medical Cannabis Use Among Individuals with SCI
A relatively large percentage of individuals with chronic SCI appear to use medical cannabis on a regular basis. 22.5% of individuals in the study reported using medical cannabis at least monthly to relieve pain (70.4%) and spasticity (46.3%). Of those 54 participants, 52.7% were daily users. The sample population were 244 adults living in the U.S. with chronic SCI sustained at least 5 years prior, with neurogenic bladder and bowel.
Article Citation: Drossel C, Forchheimer M, Meade MA. Characteristics of Individuals with Spinal Cord Injury Who Use Cannabis for Therapeutic Purposes. Topics in Spinal Cord Injury Rehabilitation. 2016;22(1):3-12. doi:10.1310/sci2201-3. (Open Access)
Racial differences in the severity of hospitalizations after a spinal cord injury: An analysis of returns to the hospital 1- 5- and 10- years after SCI for Black, White, and Hispanic Americans
It’s been noted that over a 10 year period, 93 percent of individuals with SCI will experience at least one adverse health condition requiring medical attention. This long-term analysis led by IDEAL RRTC researcher Elham Mahmoudi, Ph.D. found that ten years after traumatic injury, Black individuals had significantly longer lengths of hospitalizations, compared to Whites and Hispanics.
In an adjusted statistical model using available long-term data from the 2011 Spinal Cord Injury Model Systems:
-
One year after SCI, Hispanics were significantly less likely to have returned to the hospital, when compared to White and Black individuals in the SCI. Five years after SCI, the probability of re-hospitalization for Hispanic continued to be significantly lower than Whites or Blacks.
-
Ten years after SCI, Black individuals with SCI had been hospitalized for a significantly longer period of time, on average, when compared to Whites and Hispanics.
-
Additionally, individuals who were younger, more educated, employed, and had less severe impairments after their SCI were significantly less likely to become hospitalized at any of the 3 postinjury time points examined
The authors note, “Although not always statistically significant, at all postinjury assessment-points, Hispanic adults had the lowest and African American adults had the highest probability of hospitalization.” Together with racial differences in levels of education, unemployment, and relationship status in the study sample, the authors caution that Black Americans with SCI are less likely to access preventive health care services and have an increased chance of medical complications. They discuss a number of factors that may widen the racial differences in average length of long-term hospitalization stays: including shortcomings in care that result earlier detection of pressure sores/ulcers among White patients and later diagnosis among Black patients, requiring in more extensive treatment.
The authors conclude, “To avoid preventable hospitalization, it is important to target [preventive and rehabilitation services] services [particularly during the first year postinjury] toward more vulnerable populations, particularly African American men and those with lower incomes and education levels, who might have less social or family support to rely on during the difficult adjustment period after SCI.”
Article Citation: Mahmoudi E, Meade MA, Forchheimer MB, Fyffe DC, Krause JS, Tate D. Longitudinal Analysis of Hospitalization After Spinal Cord Injury: Variation Based on Race and Ethnicity. Archives of Physical Medicine and Rehabilitation. 2014;95(11):2158-2166. doi:10.1016/j.apmr.2014.07.399.
Resilience after SCI
Researchers analyzed survey responses from 231 individuals with SCI, as they rated their level of happiness and wrote answers to the question: “Is there anything else you would like to tell us about your resilience or ability to ‘bounce back’ when you face a challenge?”
A majority of respondents with SCI identified themselves as happy and explained their adjustment and resilience as related to personality, good social support, and a spiritual connection. Many talked about resilience and “bouncing back” after SCI and mentioned a variety of factors that either facilitated or impeded their ability to “bounce back,” including persistence, personal growth, a history of experiencing and facing adversity.
- “It is a constant battle, but after so many years you learn to bounce back quickly.”
- "It's up to me, go backwards or forward. I'm not going backwards, have to stay positive, but it is hard. But I'm alive and my 3 girls need me. I have a whole bucket of problems, so I just put a lid on it."
- "Even though the deck is stacked against me, I have to keep getting up and moving forward because other people still depend on me."
- "Wish I were younger and better physically to “bounce back.” Wish I didn't tire so easily. Chronic pain makes it hard to bounce back."
- "Felt like I was bouncing back when I had regular PT. Insurance is no longer paying."
- "The drugs used to treat my SCI have completely ruined my life. The anti-depressant used to control my nerve pain has caused severe depression that I never had before and I cannot escape from." "I still have moments of “Why me?”
Article Citation: Duggan C, Wilson C, Diponio L, Trumpower B, Meade MA. Resilience and Happiness After Spinal Cord Injury: A Qualitative Study. Topics in Spinal Cord Injury Rehabilitation. 2016;22(2):99-110. doi:10.1310/sci2202-99. (Open Access)
Follow along with the conversation this month using #SCIAwareness.